Arthroscopy is a surgical procedure by which the internal structure of a joint is examined for diagnosis and/or treatment using a tube-like viewing instrument called an arthroscope also called pinhole surgery. When performed in the outpatient setting, patients can usually return home on the same day otherwise 1-2 day admission is sufficient for all the procedures done by this technique.
The technique of arthroscopy involves inserting the arthroscope, a small tube that contains optical fibers and lenses, through tiny incisions in the skin into the joint to be examined. The arthroscope is connected to a video camera and the interior of the joint is seen on a television monitor. The size of the arthroscope varies with the size of the joint being examined. For example, the knee is examined with an arthroscope that is approximately 5 millimeters in diameter. Smaller arthroscopes also available.
If procedures are performed in addition to examining the joint with the arthroscope, this is called arthroscopic surgery. Usually causes less tissue trauma, results in less pain, and promotes quicker recovery.
Mostly after clinical examination & X-Ray; MRI findings are very helpful in assessment of pathology. But it is important to mention that MRI findings can have a percentage of error.
Arthroscopy is essentially a very low blood loss procedure and has very few complications. The underlying health of the patient is considered when determining who is a candidate for arthroscopy. Most importantly, the patient should be able tolerate the anesthesia that is used during the procedure. A person's heart, kidney, liver, and lung function should be adequate. If there are existing problems such as heart failure or emphysema, these should be optimized as possible prior to surgery. Patients who are on anticoagulants (blood thinners) should have these medications carefully adjusted prior to surgery. Other medical problems should also be controlled prior to surgery, such as diabetes and high blood pressure. Preoperative evaluation of a patient's health will generally include a physical examination, blood tests, and a urinalysis. Patients who have a history of heart or lung problems and generally anyone over the age of 50 will usually be asked to obtain an electrocardiogram (EKG) and a chest X-ray. Any signs of ongoing infection in the body usually postpones arthroscopy, unless it is being done for possible infection of the joint in question.
The patient will check into the facility where the procedure is being performed and an intravenous line (IV) established in order to administer fluids and medication. The type of anesthesia used varies depending on the joint being examined and the medical health of the patient. Arthroscopy can be performed under a general anesthetic, a spinal or epidural anesthetic, a regional block (where only the extremity being examined is numbed), or even a local anesthetic. If a general anesthetic is not used, the patient is often sedated.After adequate anesthesia is achieved, the procedure can begin. An incision is made on the side of the joint to be examined and the arthroscope is inserted into the incision. Other instruments are sometimes placed in another incision to help maneuver certain structures into the view of the arthroscope. In arthroscopic surgery, additional instruments for surgical repairs are inserted into the joint through additional small incisions in the joint. These instruments can be used to cut, remove, and suture (sew) damaged tissues. Once the procedure is completed, the arthroscope in removed and the incisions are sutured closed. A sterile dressing is placed over the incision and a brace or ACE wrap may be placed around the joint.
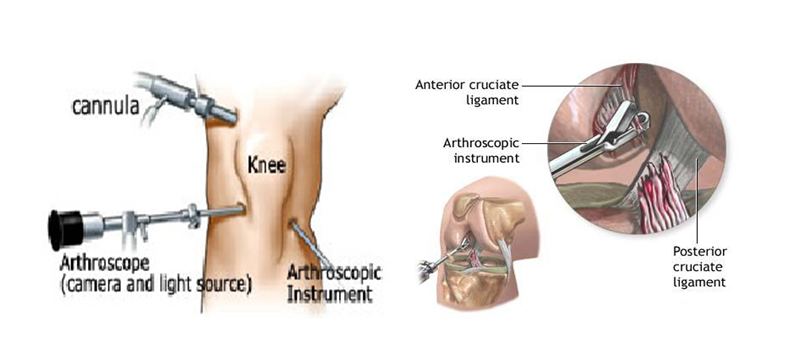
Knee arthroscopy is surgery that uses a tiny camera to look inside your knee. Small cuts are made to insert the camera and small surgical tools into your knee for the procedure.
Three different types of pain relief (anesthesia) may be used for knee arthroscopy surgery:
A cuff-like device may be put around your thigh to help control bleeding during the procedure.
The surgeon will make two or three small cuts around your knee. Salt water (saline) will be pumped into your knee to inflate the knee.
A narrow tube with a tiny camera on the end will be inserted through one of the cuts. The camera is attached to a video monitor that lets the surgeon see inside the knee.
The surgeon may put other small surgery tools inside your knee through the other cuts. The surgeon will then fix or remove the problem in your knee.
At the end of your surgery, the saline will be drained from your knee. The surgeon will close your cuts with sutures (stitches) and cover them with a dressing. Many surgeons take pictures of the procedure from the video monitor, You may be able to view these pictures after the operation so that you can see what was done.
Usually for small procedures like meniscal tears recovery is fest & 1 to 2 weeks are enough for ligament reconstructions ACL/PCL partial weight bearing walk 3 weeks & full weight bearing 6 weeks outcomes usually gratifying.
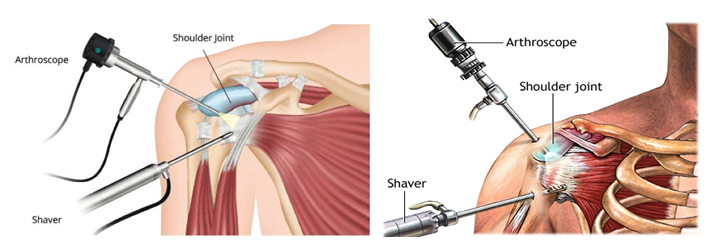
Shoulder arthroscopy is surgery that uses a tiny camera called an arthroscope to examine or repair the tissues inside or around your shoulder joint. The arthroscope is inserted through a small cut (incision) in your skin.
The rotator cuff is a group of muscles and their tendons that form a cuff over the shoulder joint. These muscles and tendons hold the arm in the shoulder joint and help the shoulder move in different directions. The tendons in the rotator cuff can tear when they are overused or injured.
You will likely receive general anesthesia before this surgery. This means you will be asleep and unable to feel pain. Or, you may have regional anesthesia. Your arm and shoulder area will be numbed so that you do not feel any pain. If you receive regional anesthesia, you will also be given medicine to make you very sleepy during the operation. During the procedure, the surgeon:
Your surgeon may need to do mini open or open surgery if there is a lot of damage. Open surgery means you will have a large incision so that the surgeon can get directly to your bones and tissues.
Preparation
Preparation of surgery is generally like another surgery.
Follow any discharge and self-care instructions you are given.
Recovery can take 1 to 3 months. You will probably have to wear a sling for the first week. If you had a lot of repair done, you may have to wear the sling longer.
You may take medicine to control your pain.
When you can return to work or play sports will depend on what your surgery involved. It can range from 1 week to several months.
Physical therapy may help you regain motion and strength in your shoulder. The length of therapy will depend on what was done during your surgery.
Arthroscopy often results in less pain and stiffness, fewer complications, a shorter (if any) hospital stay, and faster recovery than open surgery.
If you had a repair, your body needs time to heal, even after arthroscopic surgery, just as you would need time to recover from open surgery. Because of this, your recovery time may still be long.
Surgery to fix a cartilage tear is usually done to make the shoulder more stable. Many people recover fully, and their shoulder stays stable. But some people may still have shoulder instability after arthroscopic repair.
Using arthroscopy for rotator cuff repairs or tendinitis usually relieves the pain, but you may not regain all of your strength.
Hip arthroscopy is not as commonly used procedure as knee & shoulder is initially used for the diagnosis of unexplained hip pain, but is now widely used in the treatment of conditions both in and outside the hip joint. The most common indication currently is for the treatment of femoroacetabular impingement (FAI) and its associated pathologies. Hip conditions that may be treated arthroscopically also includes labral tears, loose / foreign body removal, hip washout (for infection) or biopsy, chondral (cartilage) lesions, osteochondritis dissecans, ligamentum teres injuries (and reconstruction), Iliopsoas tendinopathy (or ‘snapping psoas’), trochanteric pain syndrome, snapping iliotibial band, osteoarthritis (controversial), sciatic nerve compression (piriformis syndrome), ischiofemoral impingement and direct assessment of hip replacement.